Introduction
Pyogenic granuloma is a relatively common, soft tissue tumor of oral cavity that is believed to be reactive and not neoplastic in nature.[1] Hullihen’s description in 1844 was the first case reported in English Literature, but the term ‘pyogenic granuloma’ and ‘granuloma pyogenicum’ was introduced by Hartzell in 1904.[2] The name pyogenic granuloma is a misnomer, since the condition is not associated with pus and does not represent a granuloma histologically.[3], [4] Some authors use the term lobular capillary hemangioma for this lesion.[5] The pyogenic granuloma is thought to represent an exuberant tissue response to local irritation or trauma.[1],[2],[3] The irritating factor can be calculus, poor oral hygiene, nonspecific infection, over hanging restorations, cheek biting etc. Because of this irritation, the underlying fibrovascular connective tissue becomes hyperplastic and there is proliferation of granulation tissue which leads to the formation of a pyogenic granuloma.[6] The peak prevalence is in teenagers and young adults, with a female predilection of 2:1.[1], [4] Clinically these lesions usually present as single nodule or sessile papule with smooth or lobulated surface.[7],[8],[9] These may be seen in any size from a few millimeters to several centimeters.[7],[8],[9] Pyogenic granulomas show a striking predilection for the gingiva, with interdental papillae being the most common site in 70% of the cases. They are more common in the maxillary anterior area than any other area in the mouth.[1], [7],[8],[9] They can also be seen at extragingival sites, in the areas of frequent trauma such as the lower lip, tongue and palate.[1]
Although pyogenic granuloma an be diagnosed clinically with considerable accuracy, radiographic and histopathological investigations, aid in confirming the diagnosis and treatment. Radiographs are advised to rule out bony destruction suggestive of malignancy or to identify a foreign body.[10] Various treatment modalities have been proven to be curing the lesions. Removal of the irritant and surgical excision are usual treatments. Recently, other modes of treatments are proposed, like use of Nd:YAG laser for excision,[11] flash lamp pulsed dye laser, [12] cryosurgery, electrodessication, and corticosteroid injections. These procedures are accompanied with severe bleeding and are usually messy. Though sclerotherapy is being used extensively for varicose veins, its use as a treatment modality for pyogenic granuloma is not commonly reported. We attempted sclerotherapy procedure on pyogenic granuloma because of its vascular nature and the potential response to sclerotherapy in similar other lesions.
We hereby describe the technique of treating 3 cases of pyogenic granuloma by intralesional injection of Sodium Tetradecyl Sulfate, an Egyptian Drug Authority (EDA) and Food and Drug Administration (FDA) approved detergent sclerosant. We used SETROL, manufactured by Samarth Life Sciences Pvt. Ltd. Informed consent was taken from the patients. No local anaesthesia was used during the procedure. A maximum of 0.5 ml of undiluted sclerosant was injected into the lesion till the point of blanching. After this, the lesion was compressed with a cotton gauze for 1-2 minutes. The patient was completely comfortable.
Case Report 1
A 20 year old female patient reported with a chief complaint of growth on palate since 1 month. On intra oral examination, there was a solitary, well defined, rough surfaced, sessile growth, measuring 1 cm x 1 cm, present between right maxillary 2nd premolar and right maxillary 1st molar. (Figure 1) Lesion was firm, fibrotic and non tender on palpation. The oral hygiene status was poor, with calculus deposits present. Treatment comprised of intralesional injection of 0.5 ml of sodium tetradecyl sulphate, given at the centre of the lesion. (Figure 2) Colour of the lesion was changed to dark purple, as the sclerosing action started. (Figure 3). Patient was recalled after 3 days. Lesion was completely resolved. (Figure 4). Complete oral prophylaxis was performed. A six-month follow-up visit showed no recurrence.
 | Fig : 1 Pyogenic Granuloma Seen On Palate
 |
 | Fig : 2 Intralesional Injection Of Sts
 |
 | Fig : 3 Colour Change, As The Vessel Starts Getting Sclerosed
 |
 | Fig : 4 Complete Healing Of The Lesion After A Week
 |
Case Report 2
A 35-year old male patient reported with a chief complaint of growth in right lower gums that bled profusely while brushing of teeth. The patient couldn’t recall the exact time of initiation of growth and noticed the growth 10 days back, as it was causing discomfort while brushing. Intra- oral examination revealed a shiny, rough surfaced, reddish pink, sessile growth on gingiva between the right mandibular 1st and 2nd molar region. The growth measured 2 cm x 2 cm. (Figure 5) Lesion was firm, fibrotic and mildly tender on palpation. Oral hygiene of the patient was fair. Treatment comprised of intralesional injection of 0.5 ml sodium tetradecyl sulphate, given at 2 locations of the lesion. (Figure 6) Blanching of the lesion started. (Figure 7) Patient was recalled after 3 days. Lesion was completely healed, with no residual lesion and scarring. (Figure 8) Complete oral prophylaxis was performed.
 | Fig : 5 Pyogenic Granuloma Seen On Mandibular Gingiva
 |
 | Fig : 6 Intralesional Injection Of Sts
 |
 | Fig : 7 Colour Change Of The Lesion
 |
 | Fig : 8 Complete Healing Of The Lesion After A Week
 |
Case Report 3
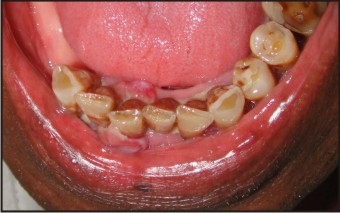
A 55 year old male patient reported with a chief complaint of enlargement of gums in relation to lower front tooth region for the past 1 year. On examination, there was a dumb bell shaped lesion in relation to 41, 42, extending from labial to the lingual aspect in relation to mandibular anterior teeth. (Figure 9,10) lesion was covered with white pseudomembrane. On palpation, the lesion was soft and vascular with a tendency to bleed. Treatment consisted of intralesional injection of labial and lingual surfaces, with 0.5 ml sodium tetradecyl sulphate. Colour of the lesion was changed to dark blue. (Figure 11) Patient was recalled after 3 days. Lesion was completely healed. (Figure 12).
 | Fig : 9 Pyogenic Granuloma Seen On Mandibular Anterior Region
 |
 | Fig : 10 Lesion Seen On Lingual Surface
 |
 | Fig : 11 Colour Change Of The Lesion After InjectionFig : 11 Colour Change Of The Lesion After Injection
 |
 | Fig : 12 Complete Healing Of The Lesion After A Week
 |
Discussion
The goal of sclerotherapy is to cause endothelial and vein wall damage in a controlled fashion. The result is removal of abnormal vessels that carry retrograde flow without damaging adjacent vessels that carry normal antegrade flow. The sclerosant effect results in a fibrous cord that is absorbed over time.[14]
The ideal sclerosant unfortunately does not exist. The available agents fall into three major categories - hyperosmolar, detergent, and chemical.[15] Hyperosmolar solutions are nonspecific in cellular destruction affecting endothelial cells as well as red blood cells through dehydration. Chemical sclerosants have a direct corrosive effect, which disrupts the intercellular cement and poisons cell surface proteins and affects chemical bonds immediately on vein wall exposure. The Detergent solutions are the most versatile and effective sclerosants available with a capacity to treat all vein sizes. Their intravascular action causes cell surface membrane disruption and extraction of cell surface proteins within seconds and its effect continues on for minutes to hours. Unique to this class of drugs is its micellular concentration, which can be enhanced with foaming. This foaming nature of detergent sclerosants results in potentially equal efficacy at lower concentrations. The best known detergent solutions worldwide are polidocanol and sodium tetradecyl sulfate (STS). The advantages of STS and polidocanol detergent
sclerosants are the absence of pain with intravascular injection and a very low incidence of allergic reactions. There is also no hemolysis as a direct effect of the drug and therefore the potential for less hyperpigmentation. The main disadvantage of STS is extravasation necrosis and ulceration.
The advantages of sclerotherapy in the patients of pyogenic granuloma are that it causes minimal discomfort to the patient, negligible blood loss, less cumbersome, minimal surgical expertise is required and above all is economical. There is no requirement of local anaesthesia or post operative dressings or any specific care.
Conclusion
Sclerotherapy with STS is effective in the treatment of pyogenic granuloma and offers an alternative to conventional methods in cases for which conservative treatment is preferable.
References
1. Nevile BW, Damm DD, Allen CM, Bouquot JE: Oral and Maxillofacial Pathology Second edition. W.B. Saunders Co; 2004:444-449.
2. Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: a review. J Oral Sci 2006; 48: 167-75.
3. Karthikeya Patil, Mahima VG, Lahari K: Extragingival pyogenic granuloma. Indian Journal of Dental Research 2006, 17:199-202.
4. Regezi JA, Sciubba , James J, Jordan Richors CK: Oral Pathology, clinical pathologic correlation Fourth edition. Sanders Company; 2003:115-76.
5. Akyol MU, Yalciner EG, Dolan AI: Pyogenic granuloma (lobular capillary hemangioma) of the tongue. Int J Pediatr Otorhinolaryngol 2001, 58:239-241.
6. Kerr DA. Granuloma pyogenicum. Oral Surg Oral Med Oral Pathol 1951; 4: 158.
7. Greenberg MS, Glick M: Burket's Oral Medicine Diagnosis & Treatment. Tenth edition. B C Decker inc; 2003:141-142.
8. Cawson RA, Odell EW: Cawson's essentials of oral pathology and medicine 7th edition. Churchill Livingston; 2002:277.
9. Eversole LR: clinical outline of oral pathology, diagnosis and treatment Third edition. B C Decker inc, Hamilton. London; 2002:113-114.
10. Maryam Amirchaghmaghi, Farnaz Falaki, Nooshin Mohtasham, Pegah Mosannen Mozafari. Extragingival pyogenic granuloma: a case report. Cases Journal 2008, 1:371
11. Hidetaka Miyazaki. Intralesional laser treatment of voluminous vascular lesions inthe oral cavity; Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 164-172
12. Joseph Niamtu III. The treatment of vascular and pigmented lesions in oral and maxillofacial surgery. Oral Maxillofacial Surg Clin N Am 2004, 16: 239–254
13. Parisi E, Glick PH, Glick M. Recurrent intraoral pyogenic granuloma with satellitosis treated with corticosteroids. Oral Dis 2006, 12: 70-72
14. Charley Levy, Louis Mandel. Sclerotherapy of the Intraoral Hemangioma. The New York State Dental Journal 2012: 19-21
15. Charles L. Dietzek. Sclerotherapy: Introduction to Solutions and Techniques. Perspectives in Vascular Surgery and Endovascular Therapy 2007, 19: 317-324
|